Diet and Osteoporosis: How Nutrition Plays a Key Role in Bone Health
Osteoporosis is a silent condition that weakens bones over time, making them fragile and more prone to fractures. It often goes unnoticed until a minor fall leads to a major injury. With increasing life expectancy, sedentary lifestyles, hormonal changes, and nutritional deficiencies, osteoporosis is becoming more common among both men and women, especially post-menopausal women. The good news is that the right diet and lifestyle choices can significantly slow down bone loss and improve bone strength.
As a Registered Clinical Dietician and Nutritionist, Geetanjali Mengi emphasizes that nutrition is not just supportive but foundational in the prevention and management of osteoporosis.
Understanding Osteoporosis
Bones are living tissues that constantly undergo breakdown and rebuilding. Osteoporosis occurs when bone breakdown exceeds bone formation, leading to low bone density. Factors such as aging, menopause, vitamin and mineral deficiencies, low physical activity, thyroid disorders, prolonged steroid use, and poor gut health can increase the risk.
A well-planned diet can help maintain bone mass, reduce fracture risk, and improve overall quality of life.
Key Nutrients for Strong Bones
1. Calcium – The Building Block of Bones
Calcium is the most essential mineral for bone health. Adults require approximately 1000–1200 mg of calcium per day, depending on age and gender. However, simply increasing calcium intake is not enough; absorption is equally important.
Calcium-rich foods include:
* Milk, curd, paneer, and yogurt
* Ragi (finger millet)
* Sesame seeds (til)
* Almonds
* Green leafy vegetables like amaranth and broccoli
* Fortified plant-based milks
2. Vitamin D – The Absorption Champion
Vitamin D helps the body absorb calcium efficiently. Deficiency is extremely common due to limited sun exposure and indoor lifestyles.
Sources of Vitamin D:
* Sunlight (15–20 minutes daily)
* Egg yolk
* Fatty fish like salmon and sardines
* Fortified foods
Supplementation may be required under professional guidance, especially in deficient individuals.
3. Protein – Strengthening the Bone Matrix
Adequate protein intake supports bone structure and muscle strength, which reduces the risk of falls.
Good protein sources:
* Pulses and dals
* Dairy products
* Eggs
* Soy and tofu
* Nuts and seeds
A balanced intake is important, as extremely high protein diets without enough calcium may be counterproductive.
4. Magnesium, Phosphorus, and Vitamin K
These nutrients play a supportive role in bone mineralization and calcium metabolism.
Include:
* Whole grains
* Nuts and seeds
* Green leafy vegetables
* Fermented foods
Foods That Can Weaken Bones
Certain foods and habits can accelerate bone loss if consumed excessively:
* Excess salt, which increases calcium excretion
* High caffeine intake (more than 2–3 cups/day)
* Carbonated soft drinks
* Excess alcohol
* Highly processed and junk foods
Balancing indulgences with nutrient-dense foods is essential for long-term bone health.
Lifestyle Factors That Matter
Diet alone cannot protect bones without the right lifestyle support:
* Weight-bearing exercises such as walking, yoga, strength training, and stair climbing help build bone density
* Adequate sleep supports hormonal balance
* Stress management helps regulate cortisol, which otherwise affects bone health
* Avoid smoking, as it directly weakens bones
Osteoporosis Across Life Stages
Bone health should be prioritized early in life. Peak bone mass is achieved by the late 20s, making childhood, adolescence, and early adulthood critical for prevention. During menopause and aging, nutrition becomes even more crucial to slow bone loss.
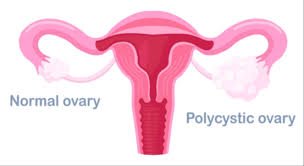
Women with thyroid disorders, PCOS, diabetes, or digestive issues need personalized nutrition plans, as these conditions can impact bone health.
The Role of a Clinical Dietician
Osteoporosis management is not about one-size-fits-all calcium supplements. A registered clinical dietician evaluates medical history, lab reports, lifestyle, gut health, and nutrient deficiencies to create a personalized plan.
Dietician Geetanjali Mengi specializes in evidence-based nutrition therapy, helping patients strengthen bones naturally while managing associated conditions like thyroid disorders, diabetes, menopause-related weight gain, and digestive issues.
Final Thoughts
Osteoporosis may be silent, but prevention doesn’t have to be. With the right nutrition, timely intervention, and professional guidance, bone loss can be slowed, fractures can be prevented, and independence can be preserved.
If you or your loved ones are concerned about bone health, seeking early nutritional guidance can make a lifelong difference. A strong foundation begins with mindful eating, balanced living, and expert support.
Geetanjali- The Voice of Healthcare- a Reg, Clinical Dietician Nutritionist, Wellness-Speaker, Author, Anchor, Wellness Expert, Pod-caster, Blogger, You tuber is based in Mumbai